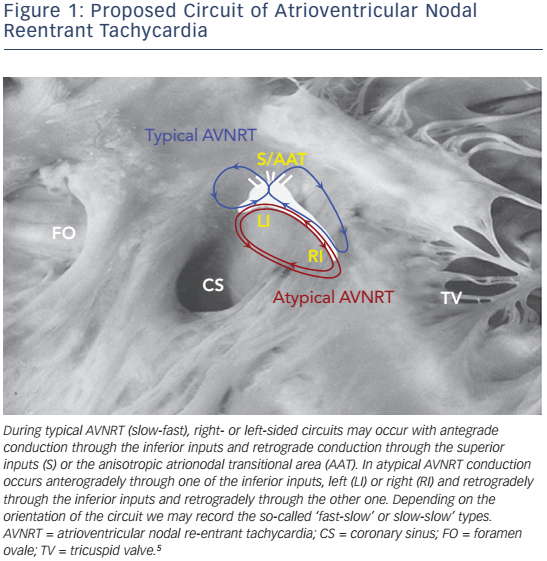
Atrioventricular nodal reentrant tachycardia (AVNRT) denotes re-entry in the area of the AV node, and represents the most common regular arrhythmia in the human.1 Although several models have been proposed to explain the mechanism of the arrhythmia in the context of the complex anatomy and the anisotropic properties of the atrioventricular (AV) node and its atrial extensions (see Figure 1),2 the actual circuit of AVNRT still remains elusive. Recent studies suggest a three-dimensional AV node with greater variability in the space constant of tissue and poor gap junction connectivity due to differential expression of connexin isoforms, that provide an explanation of dual conduction and nodal reentrant arrhythmogenesis.3,4
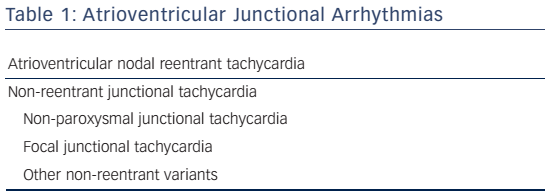
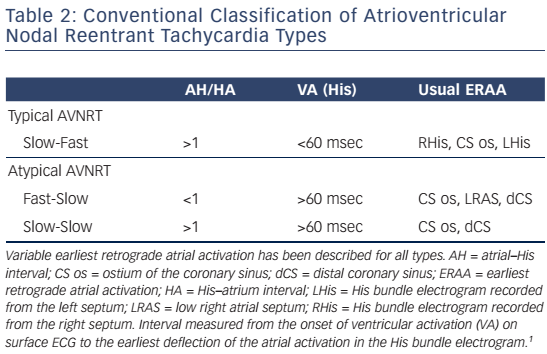
AV junctional arrhythmias are presented in Table 1. Classification schemes for AVNRT have been mainly based on the conventional concept of longitudinally dissociated dual AV nodal pathways that conduct around a central obstacle (see Table 2).
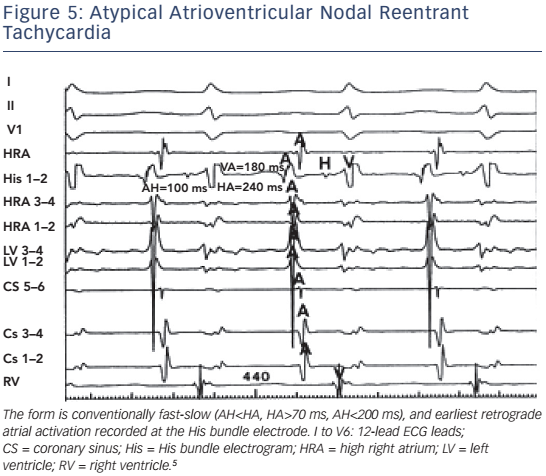
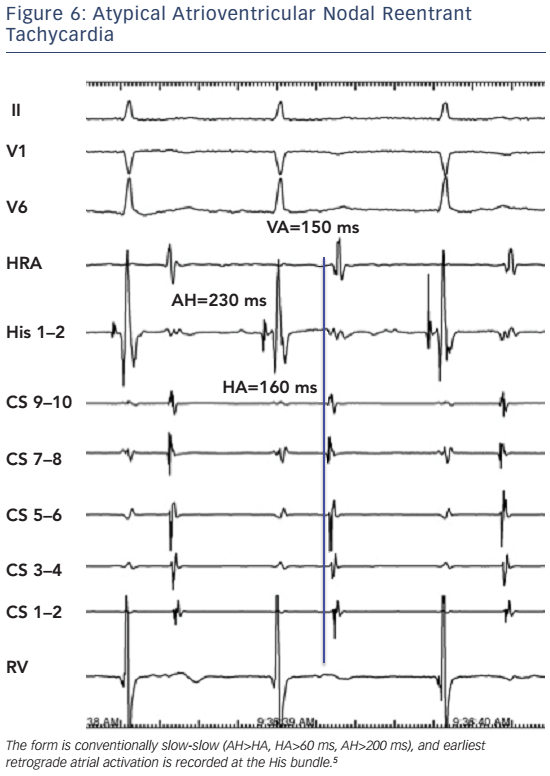
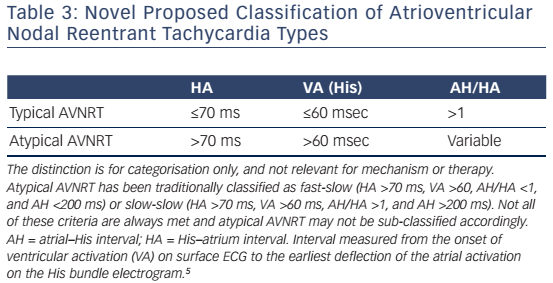
In typical slow-fast AVNRT the onset of atrial activation appears prior to, at the onset, or just after the QRS complex, thus maintaining an atrial–His/His–atrial ratio, AH/HA >1. The HA interval is usually <70 ms, measured from earliest deflection of the His bundle activation to the earliest rapid deflection of the atrial activation in the His bundle electrogram, and the VA interval, measured from the onset of ventricular activation on surface ECG to the earliest rapid deflection of the atrial activation on the His bundle electrogram, is <60 ms.1,5,6 In atypical, fast-slow form of atypical AVNRT, the retrograde atrial electrogram begins after ventricular activation with an AH/HA ratio <1. The HA interval is prolonged, ≥70 msec, and the VA interval is ≥60 msec.5,6 The atypical, slow-slow form, represents, by definition, an arrhythmia utilising two slow pathways. The AH/HA ratio is ≥1 but the HA interval is ≥70 msec, and the AH interval exceeds 200 ms.7–9
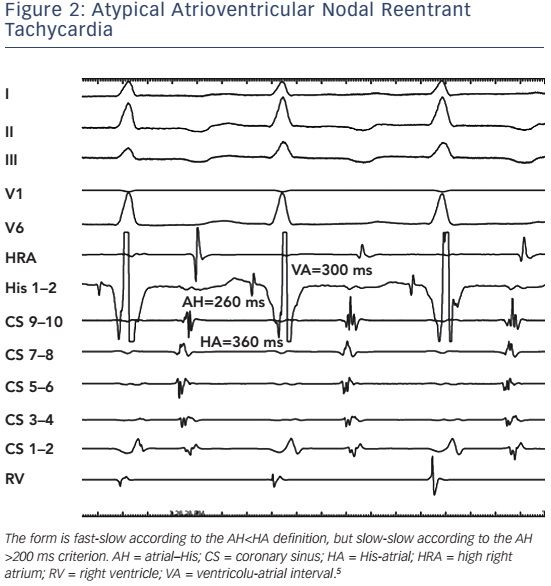
There are several inherent limitations of this classification. The distinction between fast-slow and slow-slow atypical AVNRT is often arbitrary in view of the lack of a unanimously accepted definition. In order to establish the diagnosis of a truly fast-slow form, it has been proposed that the AH interval should be less than 185 ms10 or 200 ms.6 This criterion, however, has not been adopted by other investigators.11–13 Thus, tachycardias with a relatively prolonged AH interval but an AH/ HA ratio <1 cannot be reliably classified as either fast-slow or slow-slow (see Figure 2). Furthermore, the term ‘fast-slow’ implies that the fast component of slow-fast AVNRT is the same as the fast in the fast-slow type. There is now evidence that this is not the case in patients who present with both types of tachycardia.14,15 Typical slow-fast and atypical fast-slow AVNRT appear to utilise different anatomical pathways for fast conduction. In addition, electrophysiological behaviour compatible with multiple pathways may also be seen, and in some patients, several forms of AVNRT may be inducible at electrophysiology study.
We have previously published a simplified classification scheme (see Table 2) that takes into account the shortcomings of conventional classification, and reflects evolving concepts regarding the nature of the AVNRT circuit in various forms of the arrhythmia (see Figure 1).5 AVNRT should be classified either as typical or atypical. In addition, not only the AH/HA and absolute HA intervals should be necessarily used as criteria for diagnosis of typical AVNRT. The ventriculo-atrial (VA) interval is also a practical and easily obtainable criterion, when the His bundle potential cannot be reproducibly and reliably recorded during tachycardia (see Table 3). As discussed later, retrograde atrial activation sequence or demonstration of a lower common pathway, should not be necessarily considered as reliable criteria for classification of AVNRT types.
Electrophysiological Features
Earliest Atrial Retrograde Activation
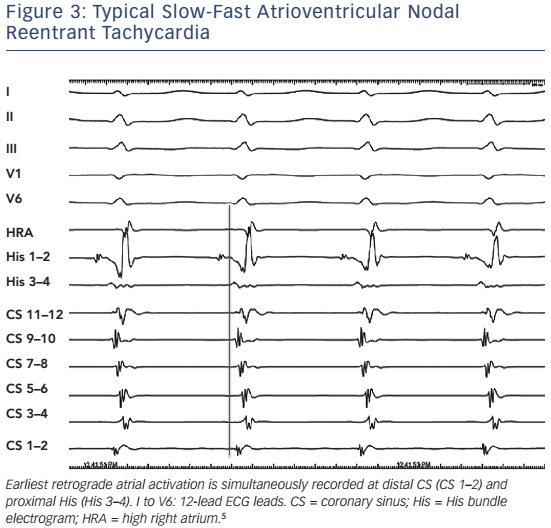
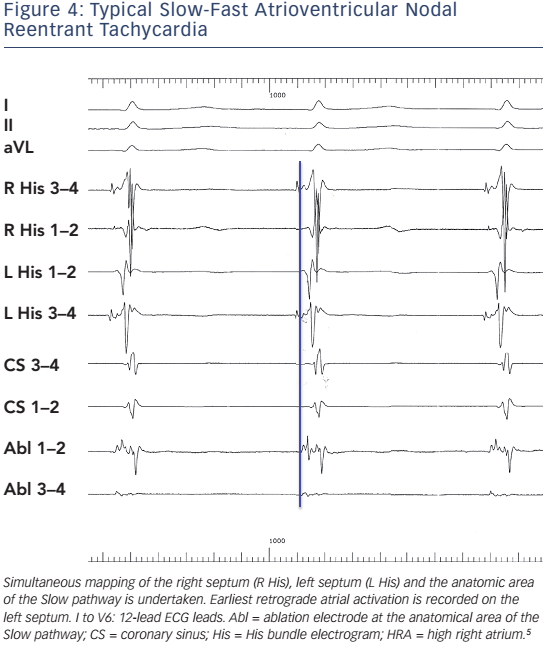
Heterogeneity of both fast and slow conduction patterns has been well described, and all forms of AVNRT may display anterior, posterior and middle retrograde activation patterns. In typical, slow-fast AVNRT, posterior or even left atrial Fast pathways may occur in ≤8 % of patients.12,13,16,17 There has also been evidence that were left septal His recordings routinely performed in patients with AVNRT, the proportion of left-sided retrograde Fast pathways might be considerably higher than previously reported.18Figure 3 and Figure 4 present typical AVNRT (slow-fast) with variable earliest retrograde atrial activation.
In atypical AVNRT, the earliest retrograde atrial activation is traditionally reported at the base of the triangle of Koch, near the coronary sinus ostium. Detailed mapping of retrograde atrial activation in large series of patients, however, has produced variable results. Earliest atrial activation can be well recorded at the coronary sinus ostium, the low right atrial septum, or the His bundle area.11–13,17 In certain cases of atypical AVNRT, retrograde atrial activation is even suggestive of a left lateral accessory pathway.8,9
It is obvious, therefore, that classification based on earliest atrial retrograde activation is inappropriate. Figure 5 and Figure 6 depicts fast-slow and slow-slow AVNRT, respectively, with earliest retrograde atrial activation at the His bundle electrode.
Relative AH/HA Intervals
The AH time and the relative AH/HA intervals have been proposed as a criterion for distinction between fast-slow and slow-slow AVNRT. However, both absolute and relative values may be meaningless in certain occasions. They depend on autonomic status, age, use of isoprenaline and sedatives and conduction properties of pathways involved, and may change during a single electrophysiology study. We have often noticed different AH/HA times in the same patient at similar or different tachycardia cycle lengths. Furthermore, when a His bundle electrogram cannot be recorded during tachycardia, a diagnosis based exclusively on them is impossible.19
Upper and Lower Common Pathways
Early studies have considered the possibility of additional AV nodal tissue extrinsic to the tachycardia circuit in order to explain various electrophysiologic phenomena observed during AVNRT,20 and the concepts of upper and lower common pathways have been longstanding controversies of AVNRT. The existence of an upper common pathway can now be rather easily refuted by subsequent evidence indicating that multiple atrial breakthroughs are extremely common,and retrograde activation often changes in timing and/or activation without significant alteration in tachycardia cycle, thus negating the notion of a simplistic focal atrial exit site.21–23 The perinodal transitional tissue is the route to the atrium, and in this context it may be considered as a common pathway of tissue but not a discrete site. The breakthrough is whatever leads to atrial activation via transitional tissue; thus there are many possibilities (see Figures 3–6).
The lower common pathway, as initially considered by Mendez and Moe, 24 has a more sound physiological basis. The notion of a lower common pathway has been utilised in order to explain phenomena of AV block without recording of a His electrogram as well as retrograde Wenckebach periodicity during AVNRT.25–28 The lower common pathway is defined as the conduction path between the distal turnaround point of the AVNRT circuit and the His bundle. The conduction time over the lower common pathway has been usually estimated by subtracting the His to atrium interval during tachycardia (measured from the onset of the His electrogram to the onset of the atrial electrogram) from that during ventricular pacing (measured from the end of the His electrogram to the onset of the atrial electrogram) at the same cycle length and considered a measurable interval in the majority of typical AVNRT cases. Initially, a lower common pathway was demonstrated in up to 75 % of 28 patients with AVNRT who were studied,20 whereas in subsequent studies with the use of para-Hisian pacing, the presence of a lower common pathway was identified in 78 % of 23 patients studied.27No evidence of a lower common pathway has been detected in typical slow-fast AVNRT.29
However, AV block during AVNRT without recording activation of the His bundle can also be explained by proximal intra-Hisian block.30 In up to one-third of patients with AVNRT the lower turnaround point of the circuit is within the His bundle, thus arguing against an intranodal circuit as a universal feature of AVNRT.31 Differences in the location of the lower turnaround sites of AV nodal reentry relatively to the His bundle have also been shown in experimental studies.32 Thus, block during AVNRT does not necessarily define a ‘lower common pathway’; it just defines longer refractory period below the circuit. This is often seen at the onset of very fast AVNRT, which may expose the His-Purkinje tissue to long-short periods and can lead to functional phase 3 block, having nothing to do with the reentrant circuit.
The electrophysiological proof of the existence of a lower common pathway depends on several assumptions that may not be valid, in a way that even if a lower common pathway exists, applied methodologies are unable to accurately detect and measure it.23 Furthermore, there are certain cases in the electrophysiology laboratory where an antegrade, let alone a retrograde, His bundle electrogram may not be reproducibly and reliably recorded.19 Thus, upper and lower common pathways seem to represent concepts the mechanism, relevance and practical applicability of which remain speculative.
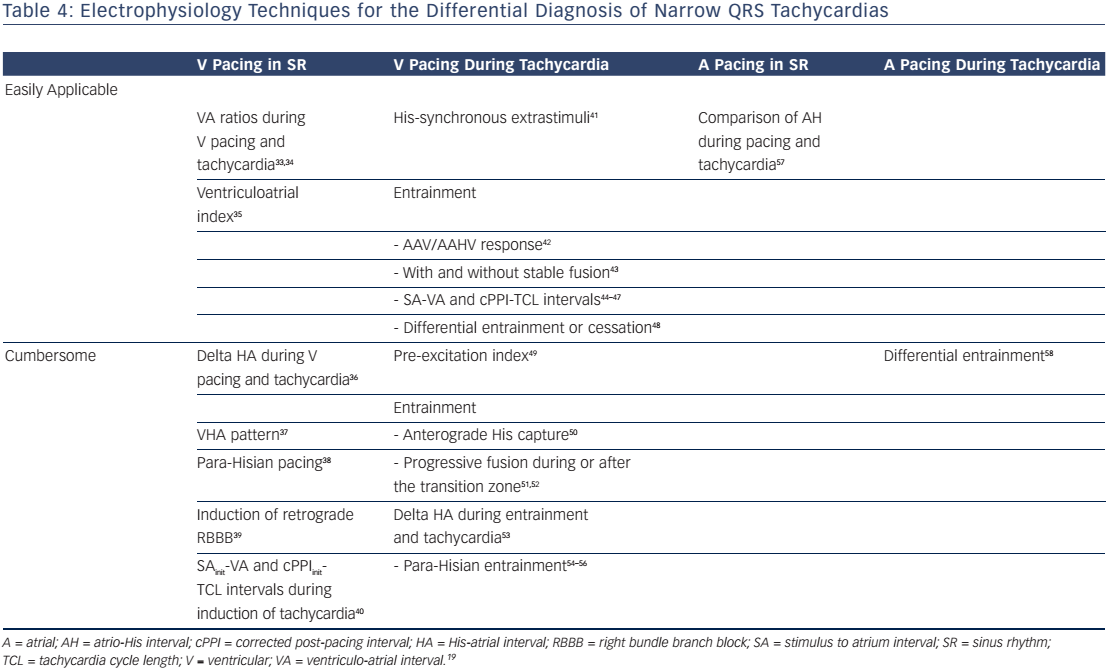
Differential Diagnosis
Differential diagnosis of a narrow QRS tachycardia, such as AVNRT, may be difficult.17 Although several ECG clues may assist differential diagnosis, this is usually accomplished at electrophysiology study and, most often, is between atrioventricular nodal reentrant tachycardia, atrioventricular reentrant tachycardia due to a concealed accessory pathway, and atrial tachycardia. Atrial and, mainly, ventricular pacing manoeuvres during sinus rhythm or tachycardia have been used with variable success rate. In clinical practice, these techniques cannot be applied to all cases, and multiple criteria have to be used for the differential diagnosis of narrow complex tachycardias with atypical characteristics. In Table 4 we summarise our experience with various techniques and manoeuvres for the differential diagnosis of narrow-QRS tachycardias in the electrophysiology laboratory.33–59
Ablation
Chronic administration of antiarrhythmic drugs (such as β-blockers, non-dihydropyridine calcium channel blockers, flecainide or propafenone) may be ineffective in up to 50 % of cases.1 Thus, catheter ablation is the current treatment of choice. Slow pathway ablation or modification is effective in both typical and atypical AVNRT. Usually, a combined anatomical and mapping approach is employed with ablation lesions delivered at the inferior or mid part of the triangle of Koch. 60,61 Multicomponent atrial electrograms or low amplitude potentials, although not specific for identification of slow pathway conduction, are successfully used to guide ablation at these areas. Ablation should be only directed towards the anatomic position of the slow pathway. If right septal attempts are unsuccessful, the left septal side should be tried.62,63
This approach offers a success rate of 95 %, is associated with a risk of 0.5–1 % AV block and has approximately 4 % recurrence rate. There is no mortality associated with this procedure.64,65 Advanced age is not a contraindication for slow pathway ablation.66 The preexistence of first-degree heart block may carry a higher risk for late AV block and slow pathway modification, as opposed to complete elimination, is probably preferable in this setting.67 Cryoablation may carry a lower risk of AV block, but it is negligible and this mode of therapy is associated with a significantly higher recurrence rate.67