Heart failure (HF) and AF share common pathophysiologic pathways and often coexist.1 Indeed, HF has been identified as the strongest predictor of AF in a Framingham Heart study population-based cohort.2 Moreover, HF and AF are involved in a vicious pathophysiological interplay. HF promotes AF mainly through raised atrial filling pressures, abnormal calcium handling, neurohormonal activation and adrenergic stimulation.3 Conversely, AF promotes HF through rapid ventricular rates, heart rate and pulse volume irregularity, and loss of left atrial kick.3
Optimal management (rate and rhythm control) of such patients is a point of debate. This subgroup is usually older and suffering from a range of comorbidities that may complicate therapeutic decisions. Meanwhile, over the last two decades catheter ablation (CA) has emerged as a treatment option for AF and has been widely utilised in clinical practice, which has been reflected in recent clinical practice guidelines.1 Congestive HF patients were under-represented in available trials on CA in AF, despite the fact that HF patients constitute a significant subset of the AF population.4 However, a range of studies have recently reported encouraging results, although there is a lack of standardisation in research protocols and result reporting. In the present article we aim to critically summarise data on CA in patients suffering from both HF and AF.
Methods
Data for this article were collected through literature searches in PubMed, and searching the clinicaltrials.gov database to identify of any ongoing studies. The search query used was: ‘ablation’ (AND) ‘fibrillation’ (AND) ‘failure’. Original articles and meta-analyses published in English reporting CA for AF in the setting of HF were considered eligible, and no publication year restrictions were applied. Additionally, the ‘snowball’ procedure was followed, i.e. references in the initially selected articles were scrutinised for identification of any other related studies. Guidelines, expert consensus documents and position statements on AF were scrutinised.
Results
Non-randomised Studies
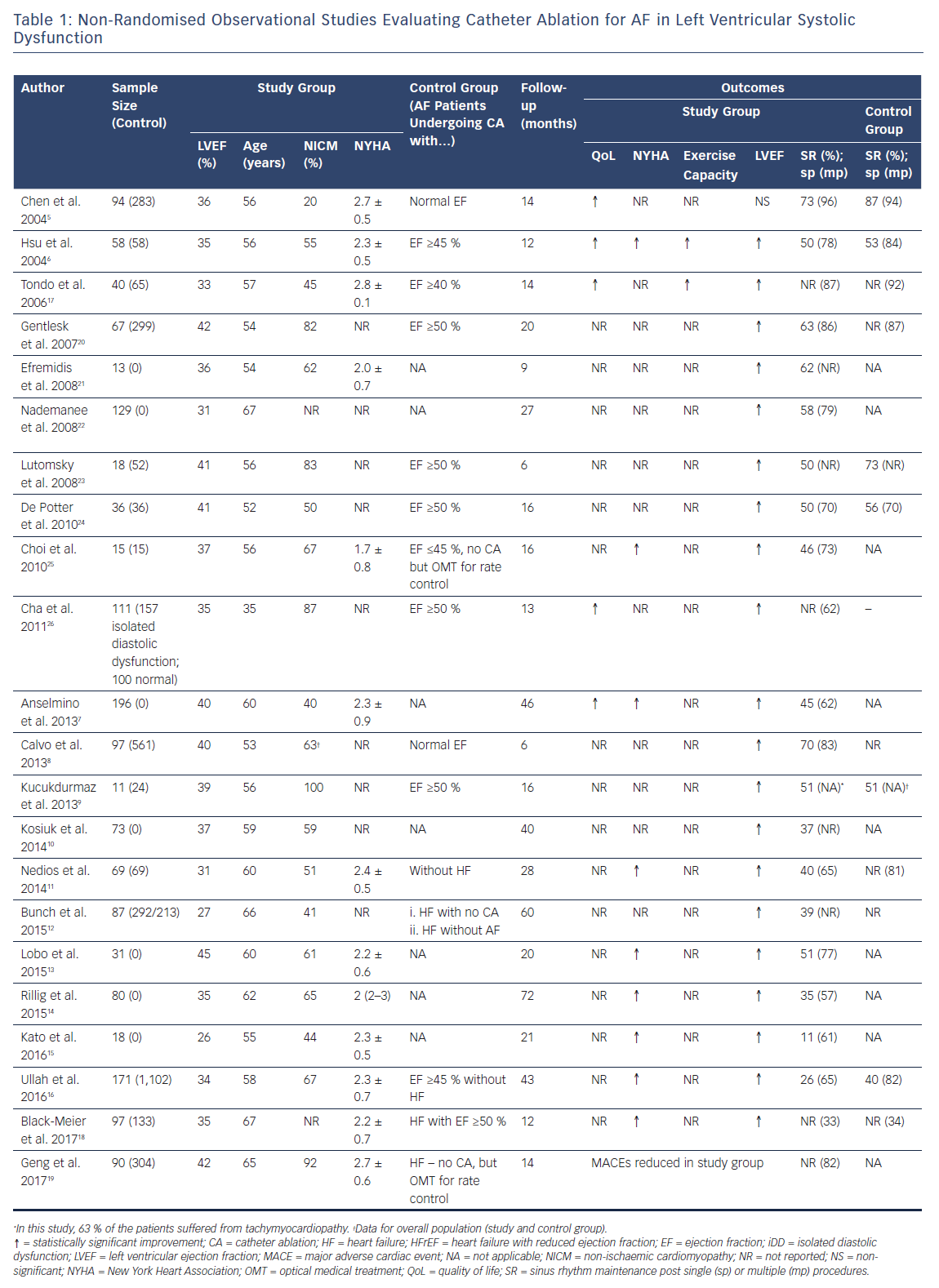
A total of 22 observational studies on CA in HF were identified, evaluating 1,601 patients and 3,763 controls.5–26 These studies provided significant data on the safety and efficacy of CA procedures in this special population, which can be considered as high risk. A marked heterogeneity in their design and choice of controls (in addition to their non-randomised design) does not allow for firm conclusions to be drawn. In most of the studies, patients with AF and HF undergoing CA were compared with patients undergoing CA for AF who did not have HF (rather than AF/HF patients treated medically). As a result, non-randomised studies have mostly addressed the issue of whether HF negatively affects CA feasibility and safety to an unacceptable extent.
The main findings of these non-randomised studies are summarised in Table 1 and will not be discussed in detail. As an overall appraisal, CA was found to be feasible and safe in patients with AF and HF. Sinus rhythm maintenance rates were quite heterogeneous, reported at a range of 26–73 % after a single procedure and 33–96 % after multiple procedures, which was not too distant from rates reported in control groups of patients with AF without HF. Additionally, post-procedural left ventricular ejection fraction (LVEF) increase as well as functional status improvement – as assessed by New York Heart Association (NYHA) classification and/or self-perceived quality of life questionnaires – were consistently observed.
Randomised Studies
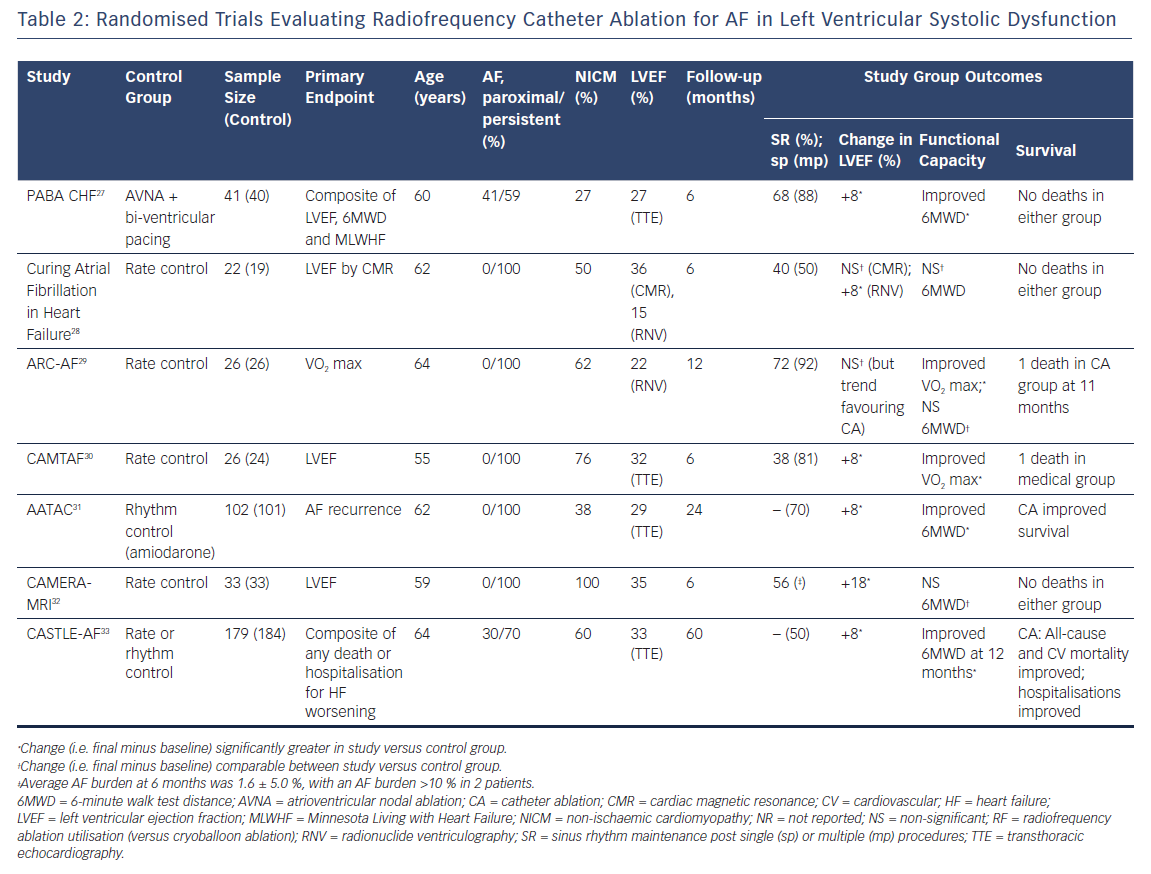
Seven randomised trials evaluating CA in HF are available to date, almost half of which are single-centre studies.27–33 All of the studies recruited patients with systolic HF, i.e. with impaired LVEF, and employed radiofrequency ablation.In four of the studies only patients with persistent AF were evaluated,28–31 while in the rest, both paroxysmal and persistent – including long-standing persistent – AF patients were included.27,33 In four studies CA was compared with rate control,27–30 while in the rest the control arm involved a rhythm control strategy or best medical treatment according to current guidelines with an effort to maintain sinus rhythm (Table 2).31,33
Pulmonary Vein Isolation versus Rate Control
Atrioventricular node ablation (AVNA) and subsequent (bi-)ventricular pacing may be perceived as an extreme form of rate control in AF management. CA is currently the cornerstone of rhythm control approaches. The Atrial Fibrillation Follow-up Investigation of Rhythm Management (AFFIRM) study and its sub-analyses implied that neither rate nor rhythm control may be considered to be a superior approach, as the beneficial effect of sinus rhythm maintenance in the rhythm control arm was essentially counteracted by anti-arrhythmic medication side-effects.34
Following this line of thought, the Pulmonary Vein Antrum Isolation versus AV Node Ablation with Bi-Ventricular Pacing for Treatment of Atrial Fibrillation in Patients with Congestive Heart Failure (PABA CHF) trial investigators evaluated CA versus AVNA plus bi-ventricular pacing with an implantable cardioverter/defibrillator in patients with AF and concomitant systolic HF.27 A total of 41 patients (60 years old; 95 % males) were treated with CA versus 40 patients (61 years old; 88 % males) treated with AVNA and bi-ventricular pacing in this randomised, multicentre, open-label study. The CA group consisted of patients with a mean LVEF of 28 %. At 6 months sinus rhythm maintenance was observed in 68 % of patients after a single ablation procedure (88 % after multiple procedures). LVEF was significantly improved in the CA group (from 27 % at baseline to 35 % at 6 months), while in the rate-control group LVEF was comparable between baseline and follow-up. Additionally, left atrial diameter, 6-minute walk distance (6MWD) and self-perceived quality of life changes also favoured CA over AVNA plus bi-ventricular pacing. Complications were comparable in the two groups. Of note, patients with non-paroxysmal AF benefited more in terms of LVEF than those with paroxysmal AF.27
A number of other small, inconclusive studies have been published. A randomised, single-centre study by MacDonald et al. found that the LVEF change at 6 months (evaluated with MRI) was comparable in the two groups.28 In the Assess Catheter Ablation Versus Rate Control in the Management of Persistent Atrial Fibrillation in Chronic Heart Failure (ARC-AF trial) LVEF improved significantly in both the CA and rate control groups, but the magnitude of change was comparable between groups.29 The Catheter Ablation Versus Medical Treatment of Atrial Fibrillation in Heart Failure (CAMTAF) trial reported an increase in LVEF in the CA group in contrast to the medical management group in which a decrease was observed, accompanied by improvements in peak oxygen consumption, brain natriuretic peptide levels, NYHA classification and self-perceived quality of life.30 Of note, the Catheter Ablation Versus MEdical Rate Control in Atrial Fibrillation and Systolic Dysfunction (CAMERA-MRI) trial, a randomised, multicentre study, evaluated CA versus rate control and reported a significantly greater improvement in LVEF (as assessed by MRI) in the CA group.32 This was accompanied by favourable outcomes in natriuretic peptides, but not in functional improvement (as assessed by 6MWD).
Pulmonary Vein Isolation Versus Anti-arrhythmic Drug Therapy
In the Ablation Versus Amiodarone for Treatment of Persistent Atrial Fibrillation in Patients with Congestive Heart Failure and an Implanted Device (AATAC) trial, Di Biase et al. investigated the effects of CA (102 patients) versus rhythm control with amiodarone (101 patients) in patients with persistent AF, dual-chamber ICD or cardiac resynchronisation therapy defibrillator in the setting of systolic HF.31 At 24 months, CA patients were arrhythmia free at a rate of 70 % (versus 34 % of the amiodarone-treated patients). Unplanned hospitalisations occurred at a lower frequency in the CA group (3.8 patients needed to treat in order to avoid one unplanned hospitalisation), while improvements in exercise capacity (6MWD) and self-perceived quality of life were greater in the CA group. Finally, a significant 24-month survival benefit was observed in the CA group (8 % versus 18 %; p=0.004).
The most recent and largest randomised study, Catheter Ablation for Atrial Fibrillation with Heart Failure (CASTLE-AF), was published in 2018 and had a primary endpoint of a composite of death from any cause or hospitalisation for worsening HF.33 In an open-label, randomised trial Marrouche et al. compared radiofrequency CA (179 patients) with best medical treatment (rate or rhythm control; 184 patients) in patients with paroxysmal (30 %) or persistent (70 %) AF and systolic HF. All patients had an ICD or cardiac resynchronisation therapy defibrillator device implanted.33 The primary study endpoint occurred less frequently in the CA group (29 % versus 45 %, respectively; p=0.006) at a median follow-up of 39 months. Aside from this primary analysis, lower total mortality was observed in the CA group (13 % versus 25 %; p=0.01), along with lower cardiovascular mortality (11 % versus 22 %; p=0.009). These benefits were accompanied by lower AF burden, LVEF improvement and 6MWD increase in the CA group.
Meta-analyses
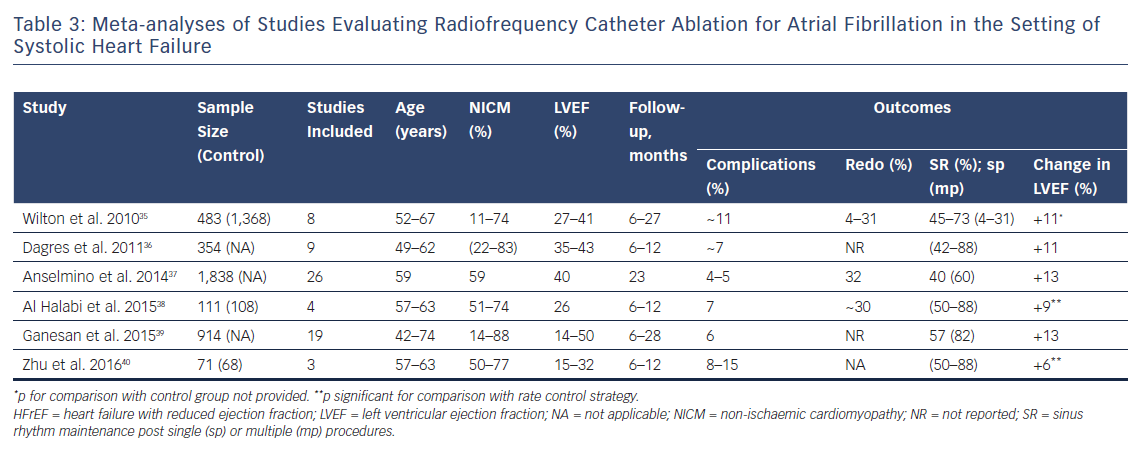
Six meta-analyses are available to the best of our knowledge; a summary of their findings is presented in Table 3.35–40 Absolute LVEF increase (in the range of +6 % to +13 %) and ‘acceptable’ sinus rhythm maintenance and procedure-related complication rates are consistent findings.
The largest meta-analytic cohort (without a control group) to date has been reported by Anselmino et al.37 The investigators included published results from observational and randomised studies evaluating CA in HF patients plus raw data from CA studies not primarily designed to evaluate, but which included, patients with HF. A total of 1,838 patients (59 years old; LVEF: 40 %; 59 % non-ischemic cardiomyopathy; follow-up 23 months) undergoing CA were included but no controls (i.e. patients treated medically) were evaluated. A significant improvement (13 % absolute increase) in LVEF was observed. Sinus rhythm (SR) maintenance after multiple CA procedures was 60 %, with 32 % of the population requiring a redo procedure. Procedure-related complications were estimated at an overall rate of 4.2 %.
While three of the available meta-analyses also report results in controls,only two of them compared patients treated with ablation versus patients treated medically.35,38,40 Both Al Halabi et al. (four studies; 111 ablation treated versus 108 medically treated patients) and Zhu et al. (three studies; 71 ablation treated versus 68 medically treated patients) concluded that ablation is superior to medical treatment in terms of LVEF and functional improvement in AF patients with depressed LVEF.38,40 Of note, these two meta-analyses included all available randomised studies at the time of their publication.
Guidelines: Consensus Documents
The most recent recommendation is the 2017 expert consensus statement on catheter and surgical ablation of AF. The experts suggest that it is reasonable that AF ablation should be offered in selected HF patients under the same criteria as if HF was not present (Class IIb; level of evidence: B-R).4
The 2016 European Society of Cardiology (ESC) guidelines for the management of AF, developed in accordance with the recent HF guidelines, make recommendations according to HF classification in HF with impaired LVEF, with mid-range LVEF and with preserved LVEF.1,41 Lack of sufficient data is underscored in the two latter categories. As far as patients with impaired LVEF are concerned, the 2016 ESC/EACTS guidelines suggest that CA may be considered in order to restore LVEF and improve quality of life without appointing a specific recommendation class. Furthermore, CA should be considered for symptom amelioration and enhancement of cardiac function when tachycardiomyopathy is suspected (Class IIa; level of evidence: B). Finally, the 2016 ESC guidelines suggest that CA for AF may be considered in patients with persisting symptoms and signs of HF, despite optimal medical treatment and adequate (ventricular) rate control in order to restore sinus rhythm and improve functional status (Class IIb-B).41
Ongoing Studies
Several studies are ongoing or have recently been completed. The Rhythm Control – Catheter Ablation with or Without Anti-arrhythmic Drug Control of Maintaining Sinus Rhythm versus Rate Control with Medical Therapy and/or Atrioventricular Junction Ablation and Pacemaker Treatment for Atrial Fibrillation (RAFT-AF) study (NCT01420393) has completed recruitment (~400 patients) and is scheduled to be completed by mid-2020. Patients with any AF type and coexistent HF have been randomised to CA and medical rate control management, and will be followed for approximately 2 years. The primary endpoint of RAFT-AF is a composite of all-cause mortality and HF hospital admission.
The Atrial Fibrillation Ablation Compared to Rate Control Strategy in Patients with Impaired Left Ventricular Function (AFARC-LVF) study (NCT02509754) was scheduled to be completed at the end of 2017, but due to procedural issues enrollment has not yet started (information provided by study investigators). In this study, 180 patients with persistent AF, LVEF ≤35 % and recent HF diagnosis were to be randomised to CA versus medical rate control treatment. The primary endpoint was a composite LVEF >35 % and a NYHA class <2 at 6 months.
The Catheter Ablation versus Medical Therapy in Congested Hearts with AF (CATCH-AF) study is expected to be completed in 2019. A total of 220 patients with systolic HF (LVEF 20–45 %) and symptomatic AF will be randomised to CA versus medical rate control and will be followed for 1 year. The primary endpoint is the time to the first of the following: hospitalisation for HF, recurrence of AF or direct current cardioversion.
Finally, the Atrial Fibrillation Management in Congestive Heart Failure with Ablation (AMICA) study was completed in mid-2017 and results are expected soon. A total of 202 patients with symptomatic AF and HF, and an indication for device implantation (implantable cardiac defibrillator with cardiac resynchronisation capabilities if appropriate) were randomised to either CA or a medical rate control strategy. The primary endpoint was LVEF at 1 year.
Discussion
Application of ablation procedures in HF patients with AF initially raised obvious concerns regarding safety and efficacy. Published data from observational and randomised studies indicated that ablation procedures in patients with AF and left ventricular systolic dysfunction were not accompanied by major safety issues. Moreover, data from the US Nationwide Readmissions Registry indicate that, in 2013, almost one in five CA procedures had been conducted in patients with AF and coexistent HF (~2,500 procedures).42 Undeniably, patients with HF may feature frailty characteristics and this should be taken into consideration in the context of a holistic patient assessment, but HF should not be considered as a contraindication. This was firmly depicted in the most recent guidelines,in which selected HF patients are expected to be treated with AF ablation for HF under the same indications as non-HF patients.4
CA success – in terms of sinus rhythm maintenance – is a major point of interest. However, rhythm control success in HF patients should only be conceived as one aspect of the potential benefits and cannot simply be defined as a total absence of AF. Improvements in LVEF, functional capacity and quality of life should also be included in the full spectrum of expected payback. Moreover, detection of the exact HF patient subsets that are expected to profit from such procedures is an as yet unattained goal.
Sinus Rhythm Maintenance
Predictors of SR maintenance after CA have drawn attention from researchers. A series of factors have been identified, but there is an ongoing debate on independent predictors of success.43 Non-paroxysmal AF (especially long-standing persistent AF) and impaired LVEF have been identified as negative predictors for success of CA regarding SR maintenance.4 However, observed SR maintenance rates after CA in AF plus HF patients who mainly suffered from persistent AF paint a noticeably less dire picture. In the available observational studies, SR maintenance after multiple CA procedures was reported at rates of 33–96 % (follow-up: 6–72 months), while in randomised studies rates of 50–88 % have been reported (Tables 1 and 2). These results are largely comparable with the reported rates of SR maintenance after CA in the general AF population4.
Left Ventricular Ejection Function Improvement
LVEF improvement after CA for AF in HF patients appears to be a consistent finding in both observational and randomised studies. All but one of the observational studies reported improved LVEF after CA procedures (Table 1). Four out of five available randomised studies that compared CA versus rate control (in patients with AF and concurrent HF) showed a beneficial effect of CA (over rate control) in LVEF; of note, the fifth study showed a statistical trend in line with the rest.27–30,32 In favour of CA was also the comparison with rhythm control (under amiodarone; AATAC trial) and the comparison with medical management including rate and/or rhythm control (CASTLE-AF trial).31,33
Finally, both available meta-analyses that provide a direct comparison of post-procedural change in LVEF after CA versus a rate control strategy show a beneficial effect on LVEF.38,40 LVEF improvement may well be attributed to the disruption of AF-related mechanisms that provoke and/or worsen HF (tachycardia, loss of atrial systolic function, ventricular rate irregularity, activation of neurohormonal pathways, and so on).3 In addition, these recent results indicate that our thus far established notion of ablation success is challenged by the fact that reduction in AF burden may in fact be more relevant in terms of prognosis compared with a traditional approach of a binary success/failure outcome. To put it simply, the detrimental effects of AF may well be alleviated through the reduction of AF burden, even in the cases of failure to achieve permanent sinus rhythm maintenance. One should also not overlook the potentially beneficial effects that may arise from withdrawal of anti-arrhythmic drugs after CA.37
LVEF improvement in patients with systolic HF could possibly lead to a reduction in the proportion of patients in whom device therapy (implantation of ICDs and/or cardiac resynchronisation devices) is indicated.44 Finally, it should be noted that patients suffering from impairment of systolic left ventricular function as a result of tachymyocardiopathy are a discrete patient subset, although it may be initially difficult to classify them correctly at the time of first diagnosis – especially when AF and impaired systolic function are diagnosed simultaneously. These patients are expected to benefit the most from CA procedures and are likely to restore normal or near-normal LV function.3,44
Functional Improvement
Another advantage of CA treatment in systolic HF patients is improvement in functional capacity and self-perceived quality of life. While there is a lack of standardisation regarding patient functional assessment in the available studies, such data are frequently reported (NYHA classification, maximal oxygen consumption at peak exercise, 6MWD, quality of life indices). Available data from randomised and observational studies (Tables 1 and 2) are concordant in terms of the improvement in functional/exercise capacity and self-perceived quality of life after CA. Indeed, randomised trials (Table 2) indicate an additive benefit of CA over rate control or medical management (rate and/or rhythm control).
Survival: Major Adverse Cardiac Events
Most available studies were not powered to assess the effect of CA on survival and major adverse cardiac events (MACEs). However, available data are promising. In a retrospective, multicentre study by Geng et al., CA (versus rate control) in systolic HF was found to reduce MACEs mid-term (14 ± 5 months) in the CA group (hazard ratio 0.51; 95 % CI [0.32–0.82]; p=0.005), although it did not affect overall survival.19 In the recent, randomised CASTLE-AF trial, the composite of any death or hospitalisation for HF worsening was reduced in the CA group (versus optimal medical management) in patients with systolic HF, while total and cardiovascular mortality were also reduced.33
Finally, the preliminary findings of the Catheter ABlation Versus ANti-arrhythmic Drug Therapy for Atrial Fibrillation (CABANA; NCT00911508) trial were announced in early 2018, but the full results have not been published (the oral presentation slides are available at www.cabanatrial.org). CABANA, when published, will be the largest (approximately 1,000 patients in each arm) randomised, multicentre trial to date with a 5-year follow-up to compare CA approach versus state-of-the-art (i.e. rate or rhythm) medical treatment.
Despite its size, randomisation and choice of a clinical endpoint, certain flaws have already been pinpointed, including a large crossover percentage between randomisation arms and a change in the primary endpoint after initiation of the study. The primary endpoint was the composite of all-cause mortality, disabling stroke, serious bleeding or cardiac arrest. On the primary intention-to-treat analysis the study results were neutral, whereas the as-treated results were in favour of CA. Still, it should be noted that these results refer to a general population of AF patients, irrespective of systolic function. In these preliminary results there was a tendency for better outcomes in patients with HF, but the interaction with HF status was apparently non-significant. Therefore, the publication of final results as well as post-hoc analyses will be eagerly awaited.
Complications: Readmissions
According to available data, CA in HF is a relatively safe procedure. Procedure-related complications are reported at rates of 3–15 % (Tables 1–3). While some of them may be life threatening (i.e. pericardial tamponade), peri-procedural death is extremely rare.
An analysis of the US Nationwide Readmissions Registry for 2013 reported a series of interesting real-life findings.42 A total of 885,270 admissions for HF exacerbation were evaluated; 364,447 were patients with coexisting AF. As expected, AF in HF patients was found to be a factor precipitating increased 90-day readmissions due to HF exacerbation (41 % versus 38 %; p<0.0001). CA treatment in HF patients (at index admission) was found to have beneficial effects. Patients who were offered CA treatment were readmitted for HF exacerbation less frequently (28 % versus 42 %; p<0.0001). In case of readmission, patients treated with CA were observed to be hospitalised for fewer days. It is noteworthy that both complications at index admission (in which CA was conducted) and total complications (index admission and readmissions) were comparable in patients who underwent CA and suffered from HF and those who were HF free. It is relevant to note that these data are purely observational but nevertheless useful in demonstrating that CA offered to select HF patients is safe and potentially beneficial in a real-life population.
Limitations
Available studies have evaluated the effect of radiofrequency CA. Procedural variants of radiofrequency CA – i.e. isolated pulmonary vein isolation or in combination with posterior wall isolation and/or ablation of non-pulmonary vein triggers – may well be a source of heterogenicity.31,37 Moreover, there is a need for procedural simplification and standardisation in this frail population.44 Indeed, frailty as assessed with reliable indices would be of value but it is not reported in the available studies. Furthermore, radiofrequency CA procedures have been reported to be less reproducible and more centre experience and caseload dependent in comparison to cryoballoon CA.45 Participant age in available studies would be an additional issue. While HF should not be considered as a contraindication for CA, we must bear in mind that available data on CA in HF patients have been derived from populations aged 50–60 years. Extrapolation to older and more fragile patients should be done with caution. In addition, trial subjects do differ unavoidably in terms of demographic characteristics from real-life patients. Based on population studies, women should represent 36–49 % of patients with AF and 40–53 % of patients with HF.46 In the available randomised trials evaluating CA in patients with AF and HF, women were grossly under-represented (at 4–27 %). Under-representation of women in HF studies has recently been commented on in an interesting paper by Scott et al.46.
Medical treatment variations may also be a source of discrepancy. However, such variations are currently included in the standard of care and it is reasonable that studies regarding CA will unavoidably be compared to this standard, as a range of ethical issues would otherwise arise.
Finally, evaluation of the ‘real’ LVEF is a largely overlooked issue. Evaluation of LVEF under the same rhythm state at baseline and at final evaluation (i.e. sinus rhythm versus sinus rhythm or AF versus AF) is not universally possible for obvious reasons, and therefore represents a potential source of inherent systematic error of such studies.
In view of the aforementioned limitations, while initial data are encouraging, important issues remain to be cleared. Therapeutic decisions should be based upon an individualised assessment of expected benefits and procedural risks. Procedural strategy (with regards to the radiofrequency ablation approach) should also be individualised and specific algorithms have been suggested to facilitate patient management.44
Conclusions
CA for AF in systolic HF patients is a feasible and relatively safe technique. Available data suggest that, apart from sinus rhythm maintenance, patients show improvement in left ventricular systolic function, self-perceived quality of life and functional capacity (favouring ablation over medical management strategies). Limited data regarding survival in this patient population are also encouraging, but which specific subgroups of HF patients – if any – are most likely to benefit from a catheter-based intervention strategy is a matter to be determined in the future.
Clinical Perspective
- Heart failure (HF) patients with AF should be treated with the same indications as non-HF patients; pulmonary vein isolation for AF in HF patients is not accompanied by any major safety issues.
- Sinus rhythm maintenance rates in HF patients undergoing pulmonary vein isolation are largely comparable to non-HF patients.
- Functional improvement (greater than conventional medical treatment) after pulmonary vein isolation in HF patients is a consistent finding in the available literature.
- The limited available data suggest benefit in terms of hard clinical endpoints, including survival, in this population.







